HIV / AIDS
What is HIV?
HIV stands for Human Immunodeficiency Virus. It is a virus that compromises the immune system, making the body more susceptible to infections and illnesses. The virus attaches to CD4 cells (cells that provide immunity against diseases), thus rendering them ineffective in fighting infections and making the body susceptible to disease. Furthermore, the virus is replicated each time a CD4 cell multiplies, thus increasing in numbers. If not kept under control, it may cause AIDS (Acquired Immune Deficiency Disease).
How does someone get HIV?
It is spread by exposure to bodily fluids including:
- Blood.
- Semen (including pre-cum).
- Vaginal mucus.
- Anal mucus.
- Breast milk.
HIV can therefore be transmitted through oral, vaginal and anal sex. Chances of transmission from oral sex is low, but still possible if there are sores, cuts or abrasions in the mouth. Use protection or avoid getting semen in the mouth in such situations. HIV can also be transmitted from a pregnant woman to her child before or during birth, and whilst breastfeeding. The risk increases if you have another STI, use drugs, share needles, and share sex toys (without using condoms).
Myths and misconceptions on HIV
You cannot contract HIV from the following:
- Contact with unbroken skin (such as holding hands).
- Kissing someone who has HIV.
- Sharing cutlery, cups, toilets, baths, towels, swimming pools.
- Touching someone who has HIV.
- Sweat, tears, urine or faeces of someone who has HIV.
- Mutual masturbation, fingering and hand-jobs can't give you HIV. However, if you use sex toys, make sure to change condoms between partners.
- Insect bites - when an insect (such as a mosquito) bites you, it only sucks your blood - it does not inject the blood of the last person it bit.
How can I lower my risk for HIV?
Condoms and PrEP, used correctly and consistently, protect you from HIV transmission during sex. You can prevent HIV infection by practising safer sex, taking PreP, and not sharing needles or other equipment if you use drugs.
I'm concerned that I might have been exposed to HIV. What can I do?
If you are concerned that you have been exposed to HIV you might want to consider taking PEP and getting tested. You need to take PEP within 72 hours of possible exposure to prevent HIV from establishing in your body. You should refrain from sex until you get tested and receive a negative result.
My partner is HIV positive. Can I get HIV?
If your partner is HIV positive, you might want to consider PrEP for a long period of time, and have sex with a condom consistently and correctly. A person with sustained undetectable levels of HIV in their blood cannot transmit HIV to their sexual partners.
Do I have to inform my partner about HIV?
Although you might not be comfortable talking about your HIV status, it is important to disclose your status with your sex partner(s) or with whom you are sharing needles. The law in Malta states that persons living with HIV who intentionally put another person at risk of transmission can be liable to criminal penalties.
What are the symptoms of HIV?
HIV infection can be asymptomatic at first; therefore the only way to know for sure is to get tested. An earlier diagnosis ensures prevention of further harm to the body, as well as decreases the risk of passing it on to someone else.
Can HIV be cured?
HIV cannot be cured, but it can be managed with antiretroviral drugs. These work by slowing the virus from spreading through the body. They do not kill the virus. When a person is living with HIV and is on effective treatment, it lowers the level of HIV (the viral load) in the blood. When the levels are low (below 200 copies/ml of blood measured) it is referred to as an undetectable viral load. This is also medically known as virally suppressed. At this stage, HIV cannot be passed on sexually.
What is the treatment for HIV?
Typically, a combination of drugs is given, to ensure that the virus is targeted. Treatment is tailored for the individual and will probably be life-long.
Are there any side-effects of antiretroviral drugs?
Treatment is known to have some side effects, including:
- Mood changes.
- Nausea.
- Diarrhoea.
- Tiredness.
- Skin Rashes.
When should I be tested?
If you think you may be at risk of having contracted HIV:
What are tests for HIV?
- Rapid HIV Test - Rapid tests are often referred to as point-of-care tests. The test can be conducted by a nurse at the GU Clinic and the result is available within 20 minutes.
- Self-Testing - HIV self-testing allows people to take an HIV test and find out their result in their own home or other private location. It refers to a process in which a person collects their own specimen (blood or oral fluid), performs an HIV test, and interprets the result in a private setting in less than 20 minutes.
- Blood Test - A blood sample is sent to the laboratory and you will be told the result in a few days. The HIV test may need to be repeated as the virus has a 3-month incubation period and may not appear in the first test. At the GU Clinic you can discuss your concerns and receive the support you require before being tested. You will also be offered a GU screen in case there are other STIs.
No HIV test can detect HIV immediately after infection. If you think you've been exposed to HIV in the last 72 hours, talk to your doctor, go to A&E, or call the GU Clinic about post-exposure prophylaxis (PEP) immediately.
You can only be sure that you are HIV-negative if:
- Your most recent test is after the window period.
- You haven't had a potential HIV exposure during the window period (1 month). If you do have a potential exposure, then you will need to be retested.
What are the stages of HIV?
When someone gets HIV and doesn't receive treatment, they will typically progress through three stages of disease.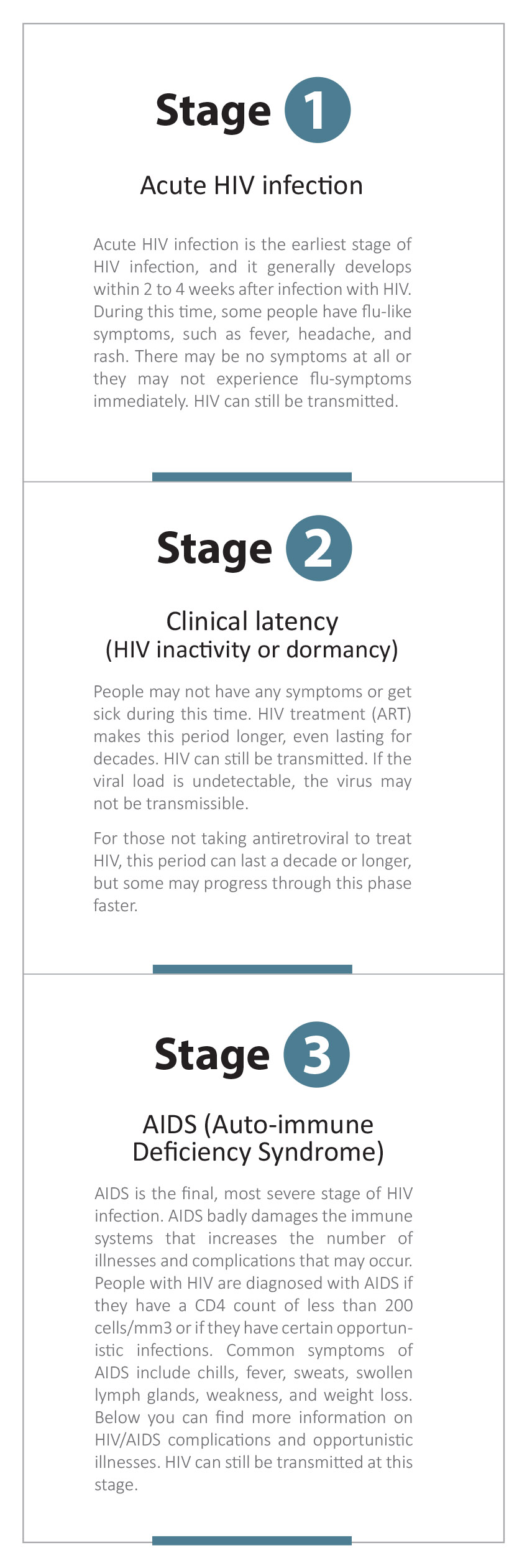 HIV and pregnancy
HIV and pregnancy
Every pregnant mother in Malta is tested for HIV during antenatal appointments and receives treatment if needed.
HIV can pass to your baby:
- During pregnancy through the placenta.
- By being exposed to the Mother's blood or other fluids during childbirth.
- During breastfeeding.
Pregnant persons with HIV should take HIV medicines during pregnancy for their own health and to prevent mother-to-child transmission of HIV.
When recommending HIV medicines to use during pregnancy, HIV specialists consider the benefits and risks of specific HIV medicines during pregnancy and for unborn babies. During childbirth, HIV medicines that pass from mother to baby across the placenta prevent mother-to-child transmission of HIV, especially near delivery.
If, at any point during your pregnancy or breastfeeding stage, you think you have been exposed to HIV, you may be able to take post-exposure prophylaxis (PEP). You need to take PEP within 72 hours of possible exposure to prevent HIV from establishing in your body and being passed on to your baby. If you're breastfeeding, you should discuss whether or not to continue breastfeeding with your healthcare professional.
Your healthcare professional will discuss with you the best method for delivery. A caesarean section is the preferred way of delivery in these circumstances.
What are the complications/opportunistic illnesses associated with HIV, for someone who does not get treated?
HIV can affect several areas in the body, for example the gastro-intestinal tract, the mouth, the eyes, the skin and the kidneys. HIV can also predispose people to viral infections and to cancer.
HIV and the Gastro-Intestinal Tract
People with HIV infection are more likely to have diarrhoea, dysphagia and odynophagia (severe pain on swallowing in the oesophagus), nausea, vomiting, weight loss, abdominal pain, anorectal disease, jaundice and hepatomegaly (enlarged liver), GI bleeding, and GI tumours (Kaposi's sarcoma and non-Hodgkin's lymphoma).
HIV and the Mouth
Mouth problems may be an early sign of HIV infection, as well as a sign of the advanced stage. The following are conditions of the mouth related to HIV:
- Oral Thrush - Candida albicans can cause oral thrush, which presents with the following symptoms: Pain in the tongue, bitter taste, sore white patches (plaques), redness and soreness on the inside of the mouth and throat, cracks at the corners of the mouth (angular cheilitis) and difficulty swallowing.
- Angular Cheilitis - This is a fungal infection that causes painful sores around the corners of the mouth, which eventually harden and form a crust. The infection can be treated with anti-fungal cream.
- Linear Gingival Erythema and Necrotising Periodontitis - These two conditions are forms of gum disease. Gum disease presents with sore bleeding gums, and rarely, periodontitis presents, where the jaw decays, causing small spaces to appear between the gums and teeth. It causes bad breath as well as difficulty swallowing and talking. If you are experiencing any of the above symptoms you should consult your physician. Good oral hygiene, as well as antibiotics and painkillers, often help. In severe cases, surgery, root planning, scaling and polishing may help.
- Stomatitis - This is a condition which causes inflammation and ulcers to appear on the mucous membranes of the cheeks, gums, tongue, lips and mouth. It is treated with antifungals.
Viral Infections
Herpes Simplex
Oral herpes can cause ulcers in the mouth which usually clear up within 7 to 10 days without treatment. However, antiviral creams may be used to facilitate healing. Most of the time the virus is inactive, and sores appear less than three times a year. However, with people who are infected with HIV, these may occur more frequently as their immunity is compromised.
Oral Hairy Leucoplakia
Oral hairy leucoplakia causes white patches with small, hair-like protrusions which usually occur on the side of the tongue. It also causes dry mouth or swelling of the salivary glands, which in turn can lead to increased risk of bacterial infection, increased acidity in the mouth, and difficulties chewing and swallowing.
As a result of oral problems, patients have difficulty chewing and swallowing food, to the extent that this substantially reduces their nutritional intake. Consequently, they are likely to show weight loss as a direct result of these problems, or stop taking their medication. However, HIV treatment will help fight mouth infections.
HIV and Warts
With HIV, the occurrence of warts is more frequent, and they are often larger and more dispersed. When presented in the genital or rectal area, they can cause discomfort. There are numerous treatment options available for warts. Warts in the genital area are often linked to cervical, rectal or anal cancer. If a person has already suffered from a genital, anal or rectal wart, regular examinations should be done.
HIV and Eye Problems
HIV retinopathy often presents in people suffering from AIDS. Cotton wool spots (white spots resulting from blocked blood vessels) and small haemorrhages are found in the retina. A more severe eye infection is CMV retinitis, caused by cytomegalovirus. It is more frequently found in people who are at advanced stages of AIDS, where the T-cell count is quite low. Symptoms include inflammation of the retina, bleeding and loss of vision. CMV can cause severe vision loss within a few months if left undiagnosed and untreated. Medication cannot cure CMV retinitis, but it can slow down the progression of the virus. A detached retina can sometimes result in CMV. This is when the retina withdraws, or detaches, from the back of the eye. This can cause severe vision loss if left untreated. Detached retina surgery is required in most cases of retinal detachments, to put the retina back in its correct alignment.
Squamous cell carcinoma of the conjunctiva is a tumour of the conjunctiva, the thin membrane that covers the white of the eye. This condition has been scientifically proven to be related to HIV/AIDS infection, infection with the Human Papilloma Virus (HPV), as well as prolonged exposure to sunlight. A variety of eye infections which can compromise vision may be more common in patients with HIV, including the herpes virus, Gonorrhea, chlamydia, toxoplasmosis, candida, pneumocystis and microsporidia.
HIV and Renal Problems
One of the common complications associated with HIV is renal disease. The adverse events of the antiretroviral medication can result in HIV nephropathy, or may result directly in kidney infection. Patients with HIV disease are also at an increased risk for developing prerenal azotaemia due to volume depletion resulting from loss of salt, poor nutrition, and nausea.
HIV and Malignancies
People with HIV are more likely to contract cancers than people not infected with HIV, and have higher incidents of anal, liver and lung cancer than the general population. Two types of cancers in particular are strongly correlated to HIV infection.
Kaposi's Sarcoma
Kaposi's sarcoma is a tumour of the blood vessels. It is more common in persons with male characteristics with HIV who have had sex with men, and is possibly caused by a herpes virus. Initially, the lesions are not painful, until they grow significantly in size. They present anywhere on the body or in the mouth, and commonly involve the legs, feet, lung, and gut. Symptoms may improve if HIV treatment is taken, however more specific treatments range from a retinoid cream, freezing, surgical removal, radiotherapy, to chemotherapy.
Non-Hodgkin Lymphoma
This is cancer of lymphocytes (white blood cells), which is marked by enlarged lymph nodes, fever, and weight loss. There are different types of non-Hodgkin lymphoma, divided into aggressive (fast-growing) and indolent (slow-growing) types. Prognosis and treatment depend on the stage and type of disease.
Managing HIV-related conditions is not just about taking medication. Getting support from family and healthcare providers, such as your GP and dentist, is important. It is also important to look after other aspects of your health, such as your weight, and by quitting smoking, controlling the amount of alcohol you consume, exercising and getting adequate rest.
Further information and help for people diagnosed with HIV
If you are HIV-positive you are seen regularly by a team of doctors at the Outpatients Clinic in Mater Dei Hospital at MOP 4 (Level -1 Medical Outpatients Block). It is important to attend every visit. If you cannot attend call in advance and ask for the nurse in charge for a re-scheduling of the appointment.
In case of any difficulty you can contact the following number:
Reference List:
https://www.cdc.gov/hiv/basics/whatishiv.html
https://www.cdc.gov/hiv/risk/index.html
https://www.ecdc.europa.eu/en/publications-data/hivaids-surveillance-europe-2017-2016-data